In-Vitro Fertilisation- Embryo Transfer (IVF-ET)
Complications
In general, the complication rate of assisted reproduction is low. These may include:
- Ovarian hyperstimulation syndrome (4%)
Signs and symptoms include abdominal distension, vomiting, ovarian cysts, fluid in the abdomen and the lungs. The worst complications are renal failure and blood coagulation problems. This might result in death. With new treatment protocols, this is rare nowadays.
Prevention
- OI/IUI cycle: use low gonadotrophin dosage to stimulate ovulation
- IVF cycle: Before stimulation, if a lot of antral follicles are seen, we use the antagonist protocol, use GnRH agonist for ovulation trigger and freeze all embryos, to be put back into the uterus during subsequent cycles.
- Multiple pregnancies (20%)
 Ovarian stimulation medicine used in assisted reproduction to produce more ovarian follicles formation will result in an increase in multiple pregnancies, which is associated with high rate of preterm labour and is undesirable for long term childhood outcome.
Ovarian stimulation medicine used in assisted reproduction to produce more ovarian follicles formation will result in an increase in multiple pregnancies, which is associated with high rate of preterm labour and is undesirable for long term childhood outcome.
Prevention
- OI/IUI cycle: use low dose gonadotrophin to stimulate ovulation. The aim is 1-3 follicles.
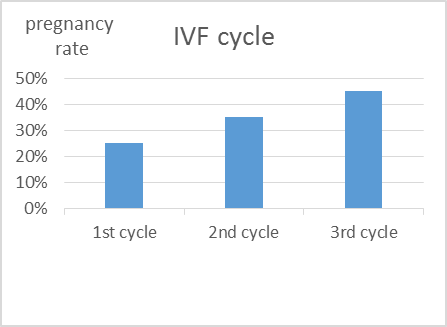
- IVF-ET cycle: Put back one embryo in each cycle. Wait till day 5 and choose one better developing embryo and do blastocyst transfer. This will improve the success rate while minimizing multiple pregnancy rates, although there is still a small chance of splitting of the blastocyst and results in monozygotic twins. The rest of the embryos would be frozen for use in subsequent cycles.
Treatment
- In case triplets occur, the patient may have to decide on fetal reduction to minimise the complications of triplet pregnancies. However, there is a 10% chance of losing all the fetuses because of the procedure.
- Surgical complications (1%)
The chance of surgical complications is low. This includes bleeding, pelvic infection and injury to the surrounding organs.
- Congenital birth defects (3-4%)
Birth defects may be a result of fertility treatment or infertility itself.
For natural conception, the prevalence of birth detect is about 3%. Recent studies showed that the increased risk of birth defects associated with IVF was no longer significant after adjustment for parental factors. The risk of birth defects associated with ICSI remained increased after multivariate adjustment. The increase can be due to the procedure or the transmission of male genetic abnormalities to the offspring (see ICSI section). However, even if there is an increase rise of 30-40% in birth defects with ICSI fetus, given a baseline of 3% of birth defects, the increase is by 1%, that is 4%. Counselling is required before treatment.
Females over 35 years of age have higher chance of chromosomally abnormal fetuses.
- Pregnancy outcome
Miscarriage (20%)
The miscarriage rate is slightly higher than the general population given the background risk of miscarriage is higher in the subfertile population.
Ectopic pregnancy(5%)
Ectopic pregnancy, i.e. pregnancy located outside the womb. Usually the ectopic pregnancy is located in the fallopian tube. This may be due to increased incidence of abnormal fallopian tubes in patients requiring IVF treatment.
Treatment can be conservative, medically with methotrexate or surgically with salpingectomy.
- Ovarian Cancer
There is No Evidence that infertility treatment will increase the incidence of ovarian cancer.