Male Infertility
Usually we do semen analysis to assess male infertility. Semen analysis remains the best test to assess the capacity of sperm to fertilise an egg. Two to three semen specimens may be required for an accurate assessment.
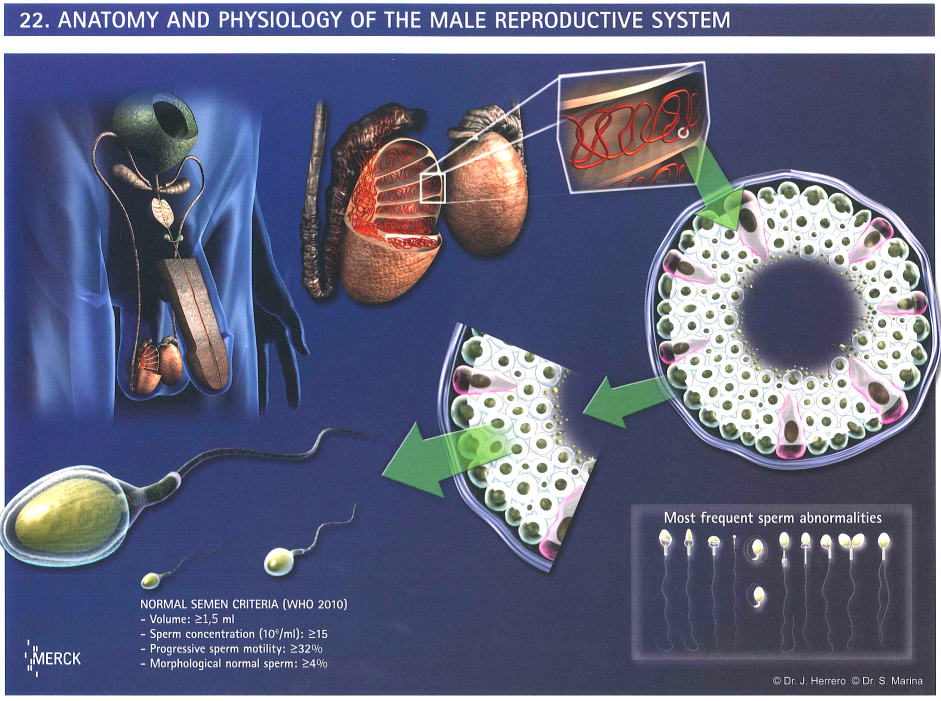
The World Health Organisation (WHO) 2010 reference values are used.
| Criteria | Lower Reference Value(5th Percentile, 95% CI) |
| Sperm Concentration | 15M/ml (12 - 16) |
| Total Sperm Number | 39M (33 - 46) |
| Total Motility (PR+NR) | 40% (38 - 42) |
| Progressive Motility (PR) | 32% (31 - 34) |
| Sperm Morphology (Normal Form, Strict Criteria) |
4% (3 - 4) |
Table: Semen Parameters from Fertile Men whose partners had a time-to-pregnancy of 12 months or less.
Men with semen parameters below the lower reference values are not necessarily infertile.
|
Male reproduction system
| |
Sperm |
Semen analysis |
Treatment modalities:
- Medicine
- - Viagra can treat ejaculatory problems
- - Gonadotrophins can treat hypogonadotrophic hypogonadism male infertility
- - Poor semen parameters are largely genetic. Clomid, testosterone and steroid treatment will not improve pregnancy rates.
- Surgery
- - For men who have had a vasectomy, reversal of vasectomy may help to restore fertility
- - For men with varicocele, varicocelectomy is controversial in improvement of pregnancy rate
- - If there is no sperm found in semen, percutaneous epidydimal sperm aspiration (PESA) or testicular sperm extraction (TESE) may be performed to retrieve sperms for IVF usage
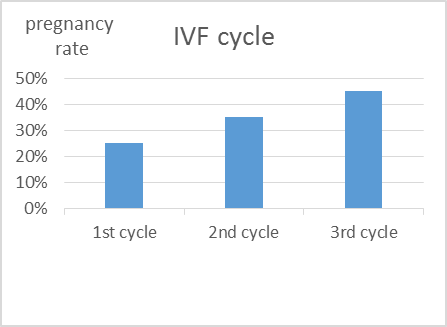
- Assisted reproductive technologies
- - IUI or IVF
- - IUI can be considered for male infertility with mild semen abnormalities
- - IVF-ET is suitable for male infertility with moderate semen abnormalities
- - IVF-ICSI-ET is suitable for male infertility with severe semen abnormalities
Treatment method of choice with regards to sperm count
| Treatment method | Least sperm count required to achieve fertilisation |
| IUI | 1,000,000 |
| IVF | 10,000 |
| IVF + ICSI | 1 |
| PESA/TESE | 0 (no sperm is found in the ejaculate) |
Most studies have shown that sperm morphology is the best indicator, as compared to concentration and motility, of fertility potential.
For sperm morphology ≤4%, the success rate with IUI is low, IVF treatment should be considered.
For severe semen parameters impairment, IVF-ICSI-ET is the most effective way in achieving pregnancy.